
Privacy statement: Your privacy is very important to Us. Our company promises not to disclose your personal information to any external company with out your explicit permission.
Tumescent liposuction (TL) is one of the most commonly performed cosmetic surgeries in the United States. Although liposuction is not a therapy for obesity, it can be used to create a more aesthetic silhouette for a given body shape. Tumescent liposuction allows for the removal of large volumes of fat with minimal blood loss, low postoperative morbidity and mortality, and excellent cosmesis. This article reviews preoperative and postoperative considerations as well as techniques to optimize treatment outcomes in various body areas.
Cutis. 2012;90:259-265.
Liposuction is the surgical aspiration of sub-cutaneous fat using cannulas introduced into the skin through small incisions. Tumescent liposuction (TL) is a technique by which the subcutaneous compartment is infiltrated with dilute concentrations of lidocaine and epinephrine, as described by Klein. By definition, TL excludes the use of other anesthetics that have risks for suppressing the respiratory system, as this procedure is performed under local anesthesia. Tumescent liposuction is an outpatient procedure that allows for the removal of large volumes of fat with minimal blood loss, low postoperative morbidity and mortality, and excellent cosmesis. It has been successfully used to contour several body areas and also can be used to correct other related noncosmetic adipose collections such as lipomas, gynecomastia, and hyperhidrosis.
Before Klein introduced TL in 1987, liposuction had been performed with en bloc resection of human fat and skin or by scraping off excess fat through skin incisions. Italian cosmetic surgeons Fischer and Fischer introduced the suction technique for fat removal in 1976, and Fournier, who is considered a pioneer in the field of liposuction, promoted syringe-assisted liposuction in 1987. Prior to the advent of tumescent anesthesia, dry liposuction, which utilizes general anesthesia with little or no local anesthesia, was the predominant method of liposuction practiced in the United States. This technique resulted in substantial blood loss and lengthy recovery times.
The introduction of tumescent anesthesia revolutionized liposuction among dermatologic and cosmetic surgeons. A 2011 survey of dermatologic procedures performed among American Society for Dermatologic Surgery members revealed that of more than 151,000 body sculpting procedures, noninvasive treatment of fat and cellulite was most common (73,900), followed by cryolipolysis (55,500) and tumescent liposuction (16,800). A remarkable safety profile, minimal blood loss, faster recovery time, and elimination of general anesthesia have made TL a favorable, affordable, and commonly performed procedure. This article will review preoperative considerations as well as techniques to optimize treatment outcomes in various body areas. Postoperative care also is discussed.
Preoperative Considerations
Consultation-When a patient first calls to schedule an appointment for a liposuction procedure, it is important for the staff member to be knowledgeable about the procedure to answer any questions the patient might ask in determining if liposuction is suit-able for his/her needs. A thorough consultation in the office should take 30 to 60 minutes.
The patient`s medical history is an important part of the consultation. Tumescent liposuction is intended for healthy adults who are within a reasonable range of their ideal body weight and have realistic expectations for results. It is important to have a low threshold for medical clearance, as some patients are unaware of their medical history and/or tend to downplay the severity of their medical conditions. Medical clearance is recommended for patients older than 60 years and for those with a history of cardiovascular disease, diabetes mellitus, and/or hypertension. Because lidocaine is metabolized by the liver, a history of hepatitis B and C virus infection, antiretroviral therapy, alcoholic liver disease, and/or chemotherapy must be considered, as they can impair liver function and cause lidocaine toxicity.
Preoperative screening studies should be performed on all patients, including a complete blood cell count, chemistry profile with liver function tests, and coagulation profile. Additionally, screening for human immunodeficiency virus and hepatitis B and C viruses also should be conducted. On the day of the procedure, a urine pregnancy test is recommended for all premenopausal women.
Recording the patient`s surgical history is an essential part of the preprocedure consultation. History of abdominal surgeries, keloids, hypertrophic scars, hernias, prior scars, and liposuction, as well as presence of postliposuction defects, should be documented; scars and defects also should be photographed with great precision.
The patient`s medication history must be complete. High-dose estrogen can put a woman at a high risk for thromboembolism within the first year following treatment, especially if she smokes. Because lidocaine is metabolized by liver enzyme cytochrome P450 (CYP450), drugs that are competitive inhibitors or inducers of this enzyme can affect lidocaine metabolism and levels in the blood. Allergies to all medications should be listed. The 2 most important drugs used in TL are lidocaine and epinephrine. Allergy to lidocaine is extremely rare; if reported, this allergy should always be taken into serious consideration. These patients should be referred to an allergist for provocative testing. More commonly, patients demonstrate allergies to methylparaben, a preservative in lidocaine. Patients with allergies to ester amides of anesthetics also are allergic to methylparaben, as the p-aminobenzoic acid cross-reacts with it. These patients should be treated with caution and should only be administered preservative-free lidocaine.
Patient Expectations-It is essential to thoroughly discuss the patient`s goals and expectations prior to the liposuction procedure to ensure his/her goals are congruent with what the procedure can accomplish. In 1998, Ozgür et al9 surveyed 3 patient populations: those seeking aesthetic surgery (n=100), those seeking reconstructive surgery (n=100), and a control group of non–surgery-seeking patients (n=100). Each group was asked to complete the socio-demographic questionnaire, life-satisfaction index, self-esteem inventory, and body-image inventory. The life-satisfaction index and body-image inventory were not significantly different in these 3 groups; however, the self-esteem inventory results were higher in the aesthetic surgery group versus the reconstructive surgery group. This finding confirms that patients seeking aesthetic surgeries are not necessarily driven by low self-esteem or other psychological issues, and their motives should be assessed individually during preprocedure consultation. Patients who combine body contouring procedures with appropriate diet and exercise regimens experience the highest satisfaction rates.
Overall, it is important for patients to have a clear understanding of which areas will and will not show improvement following liposuction procedures to ensure realistic expectations.
Tumescent Anesthesia
Since the introduction of TL in 1987, several groups have studied the safety profile of tumescent anesthesia. In 1990, Klein established a conservative guideline for the maximum dose of lidocaine used in tumescent anesthesia (35 mg/kg). He also demonstrated that peak plasma levels of lidocaine in the blood were reached at 12 to 14 hours postinfusion.
Nordströ and Ståge evaluated lidocaine plasma levels as well as objective and subjective symptoms of lidocaine toxicity for 20 hours following administration of tumescent anesthesia for abdominal liposuction, which included 35 mg/kg of lidocaine. The researchers subcutaneously infiltrated 3 liters of buffered lidocaine 0.08% with epinephrine in the abdomen of 8 female patients. The patients did not receive any intravenous fluids. Plasma lidocaine levels as well as subjective symptoms (eg, digital/circumoral paresthesia, facial fasciculation, numbness in untreated areas, lightheadedness, tinnitus) and objective symptoms (eg, nystagmus, hypertension, hypotension, arrhythmia, unnatural drowsiness) were recorded every 3 hours for a total of 20 hours. Peak plasma levels were 2.3 mg/mL and were reached 5 to 17 hours postinfusion. There was no correlation between peak plasma levels of lidocaine and dose per kilogram of body weight or total amount of lidocaine. Patients did not experience objective symptoms of fluid overload or lidocaine toxicity.
Peak plasma levels for lidocaine are achieved sooner when tumescent anesthesia is used in the head and neck areas12; therefore, TL treatment of the head and neck should not be combined with treatment of the extremities or trunk on the same day because of the rapid absorption of lidocaine from the head and neck areas. The approximate amount of tumescent anesthesia that can be infiltrated in a certain body site is briefly outlined in the Table.
Optimizing Treatment Outcomes
Abdomen-Tumescent liposuction of the abdomen provides excellent results when performed in a young nulliparous woman with toned musculature, optimum skin elasticity, and localized fatty deposits. Candidates for abdominal liposuction can be categorized into 5 groups based on fat distribution. The first group includes patients with localized fatty deposits in the lower anterior abdomen. Patients in this group typically respond well to TL and get excellent results. The second group includes patients with localized fatty deposits in the upper and lower abdomen. These patients will require liposuction in both areas, as failure to do so can result in an overhang from the upper abdomen, which may require subsequent treatment. The third group consists of patients with fat deposits in the upper and lower abdomen, flanks, and lower back. Patients who require treatment in this number of locations typically are older, postmenopausal, or have a history of weight gain. The fourth group includes patients with skin laxity, a history of weight gain and loss, multiple pregnancies, and advanced age. These patients require more liposuction than other groups but generally respond well to treatment. The fifth group includes patients with excessive skin laxity, decreased muscle tone, and localized fatty deposits. These patients see better results with abdominoplasty.
Men who desire abdominal liposuction should be evaluated with extreme caution, as some patients with abdominal protuberance have an excess of visceral fat instead of subcutaneous fat, which does not make them good candidates for liposuction. Diet and exercise might be better options for these men.
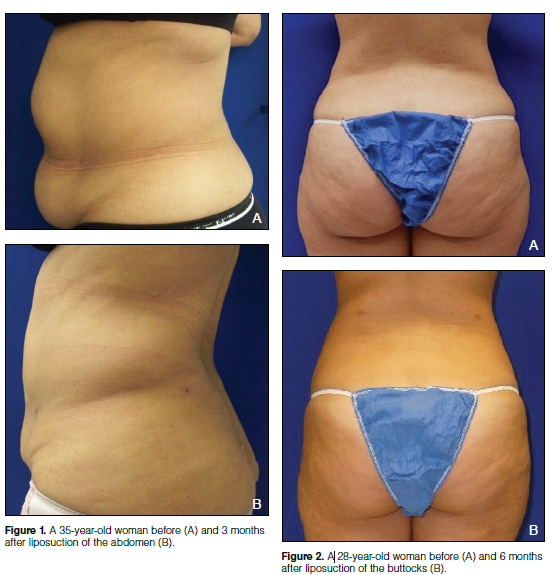
The goal of abdominal liposuction should be to reduce the bulges of fatty deposits and smooth the contour (Figure 1). A thin layer of fat underneath the skin (approximately 1 cm) should not be suctioned, as excessive suctioning can cause linear defects, dermal necrosis, and a mottled appearance of the abdominal wall.
Hips, Outer Thighs, and Buttocks-Liposuction treatment of the hips, outer thighs, and buttocks is common (Figure 2). These areas should be treated as one entity, as a disproportioned approach can result in noticeable asymmetries that will require additional treatments. When examining patients during consultation, underlying issues such as increased skin laxity, cellulite, muscle tone, prior scars, or deep defects from a prior liposuction procedure might affect the final outcome, as some of these issues might not be corrected with liposuction alone. Additionally, cultural differences in what is considered the ideal appearance of the thigh and buttock area must be kept in mind, as these expectations can vary.
Liposuction of the buttocks must be performed with extreme caution to avoid disrupting the inferior gluteal crease. When suctioning the infragluteal fat-pad, the so-called banana roll, caution also is advised to avoid ptosis of the buttocks, which is a common complication resulting from injury to the Luschka ligament. Again, it is important to set realistic expectations for the patient; bony prominences, underlying musculature, and excessive skin laxity will not improve with liposuction.
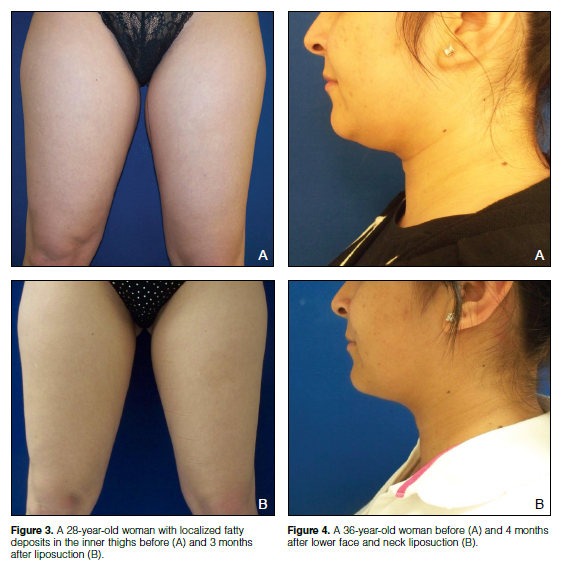
Medial Thighs and Knees-The medial thigh and knee areas often are collectively considered for treatment with liposuction, as many women have fat that extends from one end to the other. A potential pitfall in treating these areas is oversuctioning. The inner thighs are best approached when the patient is lying in a lateral decubitus position with the superomedial thighs relaxed. The inner thigh fat extends anterior, inferior, and posterior; hence, liposuction in this area must be performed in a 3-dimensional fashion
(Figure 3). If circumferential thigh liposuction is required, it is best done as a serial procedure, as there is a risk for substantial lymphostasis if treated in a single session. Oversuctioning in this area can lead to injury of the sural nerve, seroma, and reticular hyperpigmentation, which can be permanent.
Arms-Women who seek liposuction treatment of the arms typically have muscular laxity along with pendulous fatty prominence in the posterior arms. Gentle liposuction of the posterior and medial arm can create a more aesthetic shape. Liposuction of the anterior (flexural) arm should be avoided, as it can easily lead to defects.
The amount of tumescent anesthesia administered to this area should be carefully monitored, as it can lead to compartmental syndrome whereby a functional tourniquet develops distal to the infusion site, leading to fluid compression of neural, vascular, and lymphatic structures. Liposuction of the arms usually is combined with liposuction of the anterior and posterior axillary line fat-pads that can become prominent with aging. Liposuction of the axilla should be done with extreme caution, as it can affect neurovascular structures such as the brachial plexus.
Neck and Jowl-Liposuction of the neck and jowl can create youthful definition in the cervicomental angle and jawline (Figure 4). Assessing patient expectations is a key component, as combining this procedure with superficial musculoaponeurotic system plication, platysma plication, chin implant, and CO2 laser may achieve better results. An aged appearance in this area can result from a multitude of factors, including ptosis of fatty tissue and decreased elastic tissue, which can lead to a loss of the neck`s slinglike appearance, causing protuberance of the fatty tissue and loss of platysma integrity. Fullness in this area can result from multiple factors, such as excess fat; skin laxity; or low anterior placement of the hyoid bone, which can lead to an obtuse cervicomental angle. A patient with a superiorly placed hyoid bone (at the level of C3-C4 vertebrae) with jowls and submental fat would be an ideal candidate for this procedure. Asking patients to show their teeth can accentuate the platysma muscle and can help the surgeon identify patients who would benefit more from platysma plication. The ideal candidate for this procedure also has good skin elasticity, fullness of jowls, and a high-set hyoid bone with a palpable submental fat-pad. It is important to identify the position of the submandibular glands, as their ptosis can mimic jowls, which cannot be treated with liposuction.
Appropriate positioning of the patient for this procedure is with the neck slightly extended (using a neck roll pillow) in the supine position. Care must be taken to avoid excessive administration of tumescent anesthesia, which can cause compression of the trachea. After tumescent infiltration, it is best to wait at least 20 to 30 minutes to achieve adequate vasoconstriction and infusion of the tumescent anesthesia (detumescence) for easier handling of the fatty tissue during the procedure.
Entry points can be placed in the submental crease and behind the earlobes. Care must be taken to avoid injury to the mandibular branch of the facial nerve, which tends to run superficially in the jowl area. When the neck is hyperextended, the marginal mandibular nerve drops below the angle of the mandible at the anterior border of the masseter muscle. When the patient`s neck is extended, the nerve may be located as far as 2 fingerbreadths from the posterior mandibular border and becomes more superficial and more susceptible to injury. It is prudent to lift the subcutaneous fatty tissue from the underlying structures to avoid injury to the nerve and to use smaller-caliber cannulas. Suctioning lateral to the sternocleidomastoid muscle must be avoided, as there are several important neurovascular structures in the posterior neck triangle.
Male Breast-Enlargement of the male breast can be caused by fatty and glandular deposits, medications (eg, estrogen, spironolactone, digitalis, diazepam, phenytoin, clomiphene citrate), alcoholism, hypogonadism, and testicular- and adrenocorticosteroid-secreting tumors. Special attention should be paid during palpation of the breast tissue, as the presence of any lumps, hard masses, or asymmetries call for additional testing, such as mammography or biopsy.
Tumescent anesthesia is administered with an infiltration cannula or 25-gauge needle through an incision made in the inframammary crease. Following infiltration, it is important to wait for at least 20 to 30 minutes before starting the procedure to allow for adequate vasoconstriction, as the breast tissue is highly vascular. Suction typically is performed using a 16-gauge cannula for tunneling as well suctioning. Open drainage is recommended to avoid seroma formation and minimize postoperative ecchymosis.
Female Breast-Patients often seek breast reduction for several reasons, including neck, shoulder, and back pain; intertrigo; postural issues; and difficulty purchasing clothing. Traditional reduction mammoplasty is a major surgical procedure that requires general anesthesia. Patients who are not good candidates for traditional reduction mammoplasty can benefit from breast liposuction.
The amount of glandular versus adipose breast tissue is important in determining who will be a good candidate for the procedure. Women older than 40 years have a greater amount of fatty tissue than younger women who have a higher content of glandular tissue. Liposuction is only effective in the reduction of fatty tissue. Preoperative measurement of the breast adipose tissue using either a scale or water displacement method can be helpful, but several measurements are needed under standardized conditions. A family history of breast cancer is a contraindication to breast liposuction. Although there is a paucity of data showing possible difficulty in breastfeeding following traditional breast reduction, premenopausal women must be informed that there have not been any reports of this effect with breast liposuction.
After thorough tumescent infiltration, breast liposuction begins with 2 incisions: 1 in the midinframammary line and 1 in the lateral axillary line. Breast liposuction is performed in a deep plane and midplane using smaller cannulas (12- or 14-gauge cannulas). If the size of the breast is too large, serial procedures are recommended.
Although the risk for keloid scarring is high with traditional reduction mammoplasty, the risk for keloid scarring is minimal with TL. Additionally, the argument that breast liposuction can cause nipple ptosis has been firmly refuted. Breast liposuction can result in a rounded, more symmetrical breast shape.
Postoperative Care
Immediate Postoperative Care-Liposuction incisions typically are left open to drain and are not sutured. Tighter compression garments should be worn for the first 24 hours to allow adequate compression for drainage of the fluid from the incisions.
Postoperative infections after liposuction are rare; if encountered, they can be treated with oral cefazolin or clindamycin, or intravenous antibiotics depending on cultures.
In the hands of experienced surgeons, less than optimal results are sometimes seen in certain areas such as the abdomen, which may necessitate a touch-up procedure. Lawrence and Butterwick studied the number of touch-up procedures done in a large liposuction practice. In 2 years, the rate of liposuction was 12.3% among 954 liposuction surgeries. Weight gain is a major reason for repeat liposuction procedure, as 47% of their patients had weight gain.
Long-term Outcome-The biggest pitfall for long-term outcomes of liposuction is weight gain. The areas where liposuction was performed will resist weight gain and it will accumulate elsewhere. Yun et al reported increased breast size from weight gain after liposuction in the abdomen and hip area. In a patient with a small abdomen that was fine-tuned with liposuction, even minimal weight gain can increase abdominal girth because of fatty deposits that accumulate underneath the rectus abdominis muscle, thereby negating the results of the liposuction procedure.
Conclusion
Tumescent liposuction is associated with longevity of effects and high patient satisfaction. With appropriate preoperative and postoperative care as well as technique, ideal candidates will achieve a sculpted body silhouette from liposuction.
LET'S GET IN TOUCH

Privacy statement: Your privacy is very important to Us. Our company promises not to disclose your personal information to any external company with out your explicit permission.

Fill in more information so that we can get in touch with you faster
Privacy statement: Your privacy is very important to Us. Our company promises not to disclose your personal information to any external company with out your explicit permission.