
Privacy statement: Your privacy is very important to Us. Our company promises not to disclose your personal information to any external company with out your explicit permission.

Focused ultrasound has recently been developed to meet the growing demand for achieving significant non-invasive skin lifting and tightening. Photoageing of the facial tissues follows a semi-predictable progression of textural, pigmentary, skeletal, and adipose changes. Initially, dynamic rhytids are present which evolve to static rhytids with time. The tissues develop laxity, often seen in the jowls and in the submental region. Traditionally the energy delivery devices used to treat ageing skin would include ablative carbon dioxide or erbium:ytterium-aluminum-garnet (YAG) devices, or treatments such as deep chemical peels and dermabrasion. These methods rely on ablation of the dermis and reepithelialisation, whilst causing a significant enough thermal injury to the dermis in order to stimulate a wound-healing response and therefore collagen remodelling and contraction of the tissues. Unfortunately most of these treatments require significant patient downtime.
More recently, other devices have become available such as infrared and LED devices, and energy-based procedures such as radiofrequency. Radiofrequency ablation allows the use of thermal energy to the reticular dermis to cause tissue contraction and remodelling whilst minimising downtime. In addition, these have the added benefit of being a safer treatment than those listed above, for a wider range of skin types. Unfortunately the results are often more modest than more invasive procedures and there is considerable individual variation in responsiveness to treatment.
What is ultrasound?
Ultrasound is an energy modality that can be focused and penetrates deeply into the tissues to cause thermal coagulation. There are several terms used for ultrasound, such as intense focused ultrasound (IFUS), high intensity focused ultrasound (HIFU), microfocused ultrasound (MFU) and focused ultrasound (FUS). HIFU uses high-energy ultrasound and is used mainly in medical applications such as ablating tumours or adipose tissue for body contouring. MFU uses lower energy to treat the superficial layers of the skin. HIFU involves thermal and cavitation to cause cell disruption and death, whereas MFU relies on heat to achieve tissue effects. For the remainder of this article the energy modality referred to will be FUS as this is the type most commonly used in aesthetic treatments.
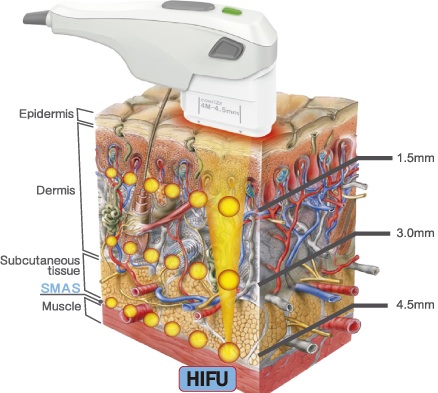
FUS is similar to the ultrasound used in medical imaging but it is highly convergent and used to form different frequencies of energy. Transducers direct the ultrasound energy to a small focal point where the elevated temperatures are capable of causing tissue coagulation. Like medical imaging, the beam of ultrasound energy can pass harmlessly through the skin allowing the focal point to target the subcutaneous tissues.
Ultrasound is the sound wave frequencies in the range of 18-20 kHz, which is above the range of human hearing. Inducible energy is delivered to specific foci in the dermis and subcutis leading to generation of heat, initiating the tissue repair cascade. Thermal coagulation points are placed at prescribed depths creating micro-coagulation zones of 1 to 1.5mm. The thermal injury is confined by keeping the pulse duration short – the epidermis is unaffected if the energy delivered is not excessive, so there is no need for epidermal cooling. As the tissue only has smaller zones of focal damage, rapid healing can occur from tissue immediately adjacent to the lesions. The ultrasound vibrates tissue and creates friction between molecules, which absorb the mechanical energy leading to heat.
Coagulation only occurs in the focal range of the beam. Energy is deposited in short pulses of 50-200 milliseconds. The energy delivered at each site is around 0.5-10J.4 It is estimated that the tissue is heated to 65-75℃ which is the temperature at which collagen denaturation occurs and tissue repair cascade begins. The intermolecular hydrogen bonds are broken causing the chains of collagen to fold and assume a more stable configuration resulting in shorter, thicker collagen. De novo collagen formation occurs in the areas of thermal tissue coagulation and new viscoelastic collagen forms causing the lifting and tightening of the skin. FUS targets the SMAS which is a fan-shaped structure covering the face and connects the facial muscles with the dermis.
The tightening seen occurs due to the heating of specific zones of tissue. Histologic evidence suggests that dermal collagen and elastic fibres were increased in number, causing thickening of the reticular dermis.5 The onset of collagen remodelling occurs up to around three months and persists for around one year, which is similar to radiofrequency or laser energy sources.
Cadaver studies have shown that penetration depth is determined by frequency – higher frequency waves produce a shallow focal injury zone and low frequency waves penetrate more deeply. They have also demonstrated consistency in depth, size and orientation of the thermal coagulation points in the subdermal soft tissue and deeper SMAS layers while preserving adjacent soft tissue. Apart from ionising radiation, ultrasound is the only type of inducible energy that can be delivered into deep tissue selectively.
Patient selection
Those who wish to avoid a surgical facelift but would like an improvement in skin laxity are ideal candidates. The patient should have mild to moderate skin and soft tissue laxity. Smokers and those with excessive photoageing are not ideal candidates as their ability to create collagen may be inadequate. Those with severe ageing, heavy and full tissues may have their result impaired by the inability of the collagen to shorten. Younger patients are more suited for the procedure as they generally have a more robust wound-healing response. Relative contraindications are medical conditions that impair wound healing and those who have a keloid response. Absolute contraindications include an open wound at the treatment site, cystic acne, a metallic implant at the site of treatment and pregnancy. Safety has been demonstrated across all skin types as absorption of ultrasound energy is independent of the melanin content of skin; the microscopic and bulk mechanical properties of the tissue determine the absorption in the skin.7
It is important that the patient has realistic expectations of the procedure. Clinical improvements are often subtle, unlike surgical procedures. There is also the potential for no appreciable clinical improvement.
Protocol
The depth of treatment is dictated by the thickness of the skin at that site. Areas with thinner skin should be treated with superficial depth and the cheek and submentum should be treated with both the deeper and superficial transducers.
In dual-plane treatment the deeper plane is treated first. The efficacy of treatment is increased when multiple treatment passes are used. In one study, areas of the face and neck were treated with a 4MHz and 4.5mm transducer followed by a 7MHz and 3mm transducer. Two blinded clinicians determined that 8 of 10 patients showed clinical improvement 90 days after treatment while nine subjects reported improvement. If the vector is varied, further improvements have been demonstrated in treatment outcome. Using the same energy output one study reported that 15 vertically orientated treatment lines in 3 and 4.5mm tissue depths produced significantly greater lifting than 15 horizontally placed lines in the opposing brows and marionette lines. Overall treatment sites receiving more treatment lines and higher energy at dual depths produced significantly greater lifting. Despite concerns about lipoatrophy with FUS, this phenomenon has not been reported in the literature so far. Although FUS typically results in microscopic coagulation, staking of pulses should be avoided and repeat treatments with some time interval would be better in terms of safety to avoid cavitation.
The patient should be advised to refrain from applying facial foundation, powders and lotions on the day of treatment if possible. All metal jewellery on the face should be removed. Those with a history of herpes simplex infection should take prophylactic anti-virals for two days before and six days after treatment. The skin is cleansed of any facial makeup or product prior to treatment and some practitioners mark the number of target columns. An ultrasound gel is applied to the treatment site and the probe is placed on the skin and activated. The entire surface area of the transducer should be applied to the skin. It may be necessary to reapply ultrasound gel during the procedure to ensure proper coupling. In some machines it is possible to visualise focal depth on the monitor in the ultrasound image, which can be aligned with the corresponding layer of the deep dermis to SMAS. Parallel arrays of ultrasound pulses are delivered. The number of lines depends on the size of treatment area. Treatment should be avoided over the thyroid gland, inside the orbital rim and over implants. Post procedure the ultrasound gel is removed and the patient is free to return immediately to their usual activities.
Pain
The amount of pain experienced varies from mild to severe and the type of pain control used varies according to physician preference. The use of 5-10mg diazepam and 50-75mg meperidine 20-30 minutes prior to the procedure has been described. Others have described topical or local anaesthesia, conscious sedation, cold compresses, high-dose non-steroidal anti-inflammatories, oral or intravenous narcotics and massage. Most patients having treatment to the mid-face and neck do not require any pain control, whereas those treated to the brow may require some due the thin tissue overlaying the frontal bone. It is my preference not to use any pain relief methods, as I am aware that the patient won`t be able to notice if you are damaging a nerve when anaesthetised.
Safety
This treatment has a good side effect profile and most side effects are temporary. Possible side effects include pain, erythema, oedema and purpura. The most distressing complication which may occur is motor nerve paralysis. Areas where the facial nerve branches are superficial are at the greatest risk such as the temporal branch of the trigeminal nerve at the temple and the marginal mandibular nerve at the jawline. Symptoms can be seen one to two hours after treatment, secondary to nerve inflammation. Resolution is seen within two to six weeks. Three of the patients studied have developed transient dysaethesia to the deep branch of the supraorbital nerve lasting three to seven days and four patients developed numbness along the mandible after cheek treatment that resolved after two to three weeks.
Summary
Focused ultrasound delivers ultrasound energy to predetermined depths to the deep dermis and subdermal tissue. Neocollagenesis and tissue contraction occurs in the months after treatment. As the energy delivered is focused precisely and adjacent tissue is spared it has a very good safety profile. More recent treatment developments have included the use of this technology on other body sites including the décolletage.
LET'S GET IN TOUCH

Privacy statement: Your privacy is very important to Us. Our company promises not to disclose your personal information to any external company with out your explicit permission.

Fill in more information so that we can get in touch with you faster
Privacy statement: Your privacy is very important to Us. Our company promises not to disclose your personal information to any external company with out your explicit permission.